Case Presentation by Katherine Shulman, MD
Chief Complaint: Difficulty swallowing
History of Present Illness: This is a 66-year-old male with no significant medical history who comes in to emergency department complaining of difficulty in swallowing beginning 3 months ago. He further describes it as a foreign body sensation in his throat and has started eating a soft diet, which he tolerates well. He reports only mild discomfort with swallowing. Also, three months ago he noticed a change in his voice. He reports a “very mild” baseline shortness of breath over the same timeframe. He denies any neck pain, chest pain, fevers, night sweats, or headaches. No recent dental procedures. Denies any URI symptoms in the past several months.
Past Medical History: none
Medications: None
Social History: Denies tobacco, alcohol, or illicit drug use.
Family History: His brother just died of laryngeal cancer two months ago.
Physical Exam:
Vital Signs: BP 145/82; HR 98; RR 16; Temp 36.8; 98% RA
General: Patient sitting semi-fowler in stretcher in no acute apparent distress, with no acute respiratory distress. Handling oral secretions well. Speaking in full sentences with a muffled voice. Resting comfortably.
Head: normocepahlic; atraumatic
Eyes: EOMI; PERRL; pink conjunctiva
Mouth: moist mucous membranes, no tongue or submandiblar swelling, good overall dental hygiene, uvula midline; significant area of swelling in the right oropharynx just posterior to the tonsil with normal appearing overlying mucosa; no erythema, exudates, ulcerations in the anterior or posterior pharynx.
Neck: Supple; trachea midline; no palpable lymphadenopathy
Cardiovascular: s1, s2; regular rate and rhythm; no murmur
Respiratory: no stridor, lungs clear to auscultation bilaterally; symmetrical chest rise and fall; no accessory muscle use
Workup: We obtained laboratory tests and a CT – Neck w/ contrast.
Questions:
1. What is the most likely diagnosis?
A. Peritonsillar Abscess
B. Nasopharyngeal Carcinoma
C. Diphtheria
D. Ludwig’s Angina
2. What is the most likely causative organism?
A. Streptococcus Species
B. Staphylococcus Aureus
C. Haemophilus Influenzae
D. Fusobacterium
3. What are the next steps in management?
A. Initial dose IV Clindamycin, discharge home w/ PO Clindamycin, and ENT f/u
B. IV Unasyn, consult ENT, medicine admit
C. IV Zosyn, consult ENT, ICU admit for compromised airway
D. Consult ENT, obtain blood cultures, medicine admit
ANSWERS:
1) A
2) A
3) B
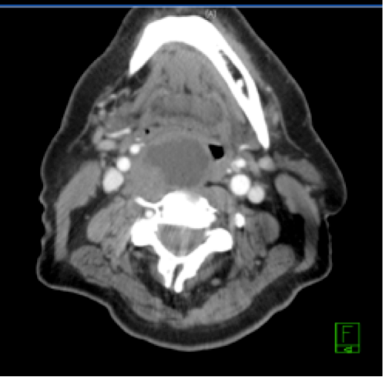
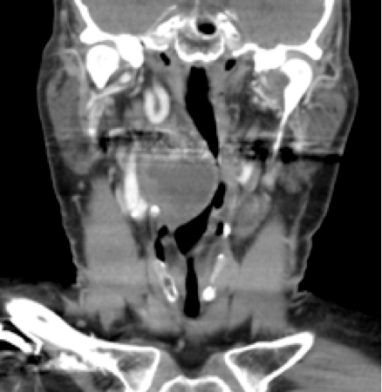
1. A. The diagnosis is right peritonsillar abscess. The CT scan shows a large peripherally enhancing complex cystic mass arising from the right peritonsillar region (best seen in the first image) causing significant mass effect. The structure measures 5.4 centimeters in the greatest dimension, and the airway measures 1 centimeter at the narrowest dimension. This is a relatively uncommon presentation of peritonsillar abscess. Usually, the progression of disease occurs within a week, signs and symptoms include: odynophagia, dysphagia, drooling, trismus, muffled voice. Additionally, fever, malaise, and dehydration are common systemic symptoms.
B. Nasopharyngeal carcinoma is uncommon in the US, difficult to detect early, and usually presents with the following: cervical lymphadenopathy, sore throat, nasal discharge or bleeding, bloody saliva, ear infection or pain, changes in hearing, tinnitus, headaches.
C. Diphtheria usually presents with an upper respiratory tract illness with sore throat, low-grade fever, and an adherent grey pseudomembrane covering the posterior aspect of the pharynx. Due to vaccinations, there has been only one case in the US in the past ten years.
D. Ludwig’s Angina is a fulminant disease process that may lead to death within hours or days. It generally occurs secondary to a dental infection, causing progressive cellulitis of the submandibular space extending to the deep tissues of the floor and mouth.
2. A. Common organisms associated with peritonsillar abscess include the following: Streptococcus pyogenes (most common aerobic), Staphylococcus aureus, Haemophilus influenzae, Neisseria species, Fusobacterium (the most common anaerobic), Peptostreptococcus, Prevotella, and Bacteroides. For most abscesses, a mixed profile of both aerobic and anaerobic organisms proliferates. The final culture in the case above was positive for Streptococcus viridans, negative for anaerobic organisms.
3. B. IV antibiotics should be started. Unasyn, Zosyn, clindamycin, a combination of penicillin G and metronidazole, are all good options for treatment of inpatient peritonsillar abscess. Mainstay of therapy is needle aspiration or incision and drainage, which in this case should be performed by ENT. The patient has a large peritonsillar abscess and an airway measuring 1 cm in diameter at the narrowest point, thus, the patient should be admitted. A medicine floor admission is an appropriate disposition. ICU is not indicated at this time, as the patient is stable and not showing signs of respiratory distress. He is neither hypoxic nor tachypneic. Physical exam demonstrates a comfortable, well appearing male. In general, peritonsillar abscesses do not take such an indolent course as described in the case above.
References:
Steyer, Terrence E. Peritonsillar Abscess: Diagnosis and Treatment. Am Fam Physician. 2002; Jan 65(1):93-97.
Marx, John A, et al. Rosen’s Emergency Medicine, 7th Ed. Philadelphia: Mosby Elsevier, 2010. Print.
Filed under: Senior Report | Tagged: ENT Cases |






Leave a comment